Healthcare data is exploding, and by 2026, it will make up more than one-third of the world’s total data. Yet, much of this valuable information remains untapped within healthcare organizations.
This comprehensive guide demystifies the healthcare data warehouse landscape for 2026, giving leaders the tools to turn raw data into better care, efficiency, and compliance.
You will learn what a healthcare data warehouse is, how its architecture is evolving, the benefits it brings, and the steps you can take to implement one effectively. Prepare your organization to thrive in the data-driven healthcare era.
Understanding Healthcare Data Warehouses in 2026
The healthcare data warehouse is at the center of modern healthcare’s digital transformation. As the volume and variety of patient information explodes, organizations need a robust system to collect, unify, and analyze this data. The healthcare data warehouse meets this need by serving as a centralized hub for information from electronic health records, lab systems, wearables, and more.
Definition and Core Purpose
A healthcare data warehouse is a centralized repository that aggregates and organizes structured data from a wide range of sources. These include EHRs, EMRs, laboratory systems, imaging, pharmacy records, and patient-generated data from wearables. The primary purpose of a healthcare data warehouse is to provide a single source of truth for healthcare organizations.
Unlike a data lake, which stores raw and unstructured data, a healthcare data warehouse is designed for structured, standardized information that supports analytics and reporting. This distinction is crucial for healthcare, where accuracy, compliance, and quick access are essential.
| Feature | Healthcare Data Warehouse | Data Lake |
|---|---|---|
| Data Type | Structured | Raw/unstructured |
| Use Case | Reporting, analytics | Exploration, data science |
| Speed of Access | Fast | Variable |
| Data Governance | High | Lower |
With a healthcare data warehouse, organizations can break down information silos and create a unified view of patient care.
Evolution of HDWs: 2020–2026
The healthcare data warehouse has rapidly evolved between 2020 and 2026. Early systems were often on-premises, rigid, and limited in scale. Today, cloud-based HDWs have become standard, offering scalability, flexibility, and real-time data processing.
One of the most significant advancements is the integration of artificial intelligence and machine learning for advanced analytics and predictive modeling. These technologies enable healthcare organizations to forecast patient risks, optimize treatment plans, and allocate resources more efficiently. The AI Integration in Healthcare Data Warehousing trend highlights how next-generation cloud data warehouses are driving personalized care and operational efficiency.
Modern HDWs also incorporate new data types, such as data from IoT medical devices, genomics, and social determinants of health. This expansion allows for more comprehensive and precise insights, pushing the boundaries of what a healthcare data warehouse can achieve.
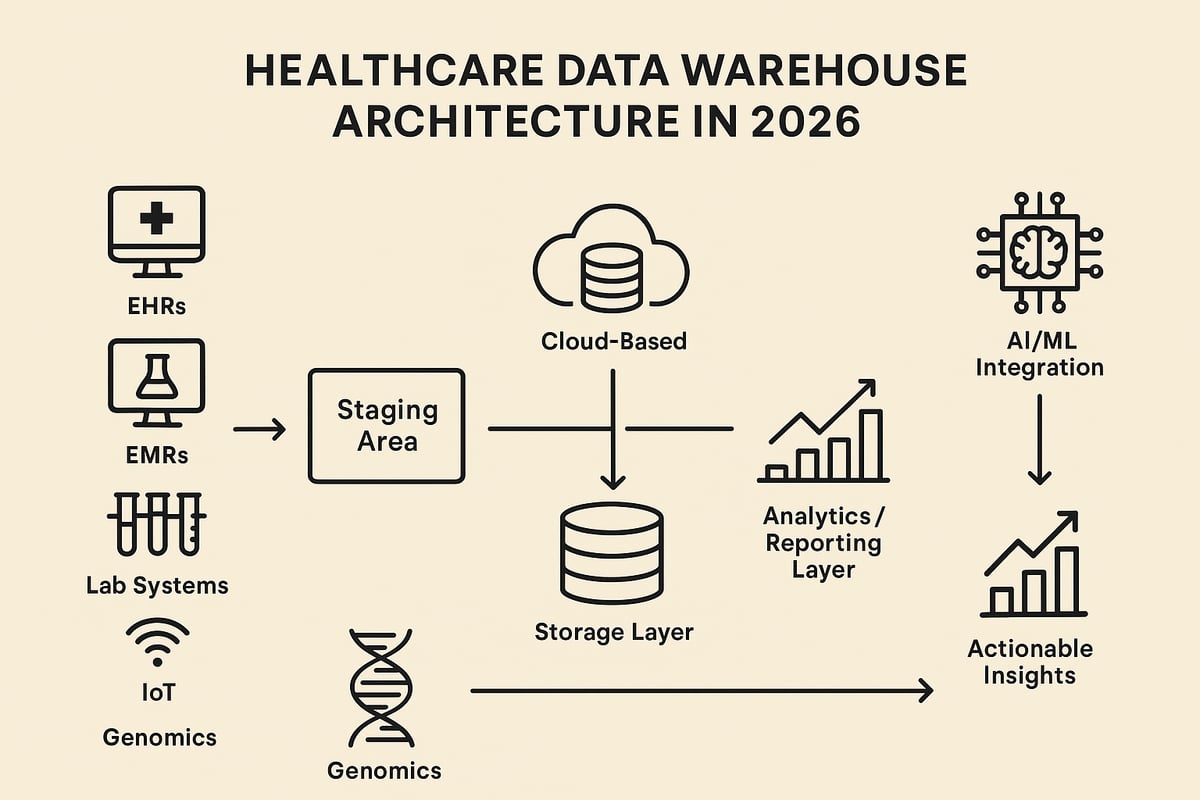
Key Components and Architecture
A modern healthcare data warehouse consists of several essential components:
- Data Sources: EHRs, insurance claims, medical imaging, pharmacy, wearables, and public health databases.
- Staging Area: Where data is transformed, cleansed, and standardized before being loaded.
- Storage Layer: Centralized storage using structured formats, often leveraging cloud infrastructure.
- Analytics and Reporting: Advanced tools and dashboards that deliver actionable insights to clinicians, administrators, and researchers.
Each layer works together to ensure that the healthcare data warehouse delivers high-quality, reliable, and accessible information.
A robust architecture supports both real-time and batch processing, allowing organizations to respond quickly to clinical and operational needs. Security, compliance, and interoperability are embedded into each layer to protect sensitive health information and support regulatory requirements.
Data Flow and Integration
The data flow within a healthcare data warehouse is a well-orchestrated process:
- Data Collection: Gather information from EHRs, lab systems, claims, and external sources.
- Staging and Cleaning: Standardize formats, validate data quality, and remove errors or duplicates.
- Enrichment: Enhance data with external datasets, such as genomics or SDoH.
- Warehouse Storage: Store structured, cleansed data for easy access and analysis.
- Analytics and Reporting: Deliver insights through dashboards, reports, and predictive models.
A critical aspect of this process is the Extract, Transform, Load (ETL) pipeline. ETL ensures that data moves seamlessly from source to warehouse, maintaining integrity and accuracy throughout. Reliable data pipelines are essential for supporting the real-time decision-making needs of healthcare organizations.
Example: Arcadia’s platform processes data from over 3,000 distinct sources, serving 170 million patient lives.
Arcadia’s healthcare data warehouse platform exemplifies the scale and complexity of modern solutions. Their system processes data from more than 3,000 unique sources, including EHRs, claims, and wearables. This enables them to serve a network covering 170 million patient lives.
By aggregating such vast and diverse information, Arcadia’s platform demonstrates how a healthcare data warehouse can support population health management, improve clinical outcomes, and drive operational efficiency. This real-world example highlights the transformative potential of advanced HDW solutions in 2026.
Key Benefits of Healthcare Data Warehousing
Healthcare organizations in 2026 face a tidal wave of data from diverse sources. A healthcare data warehouse unlocks the full potential of this information, supporting data-driven care, operational efficiency, and compliance. By turning raw data into actionable insights, organizations can transform outcomes for patients and providers alike.
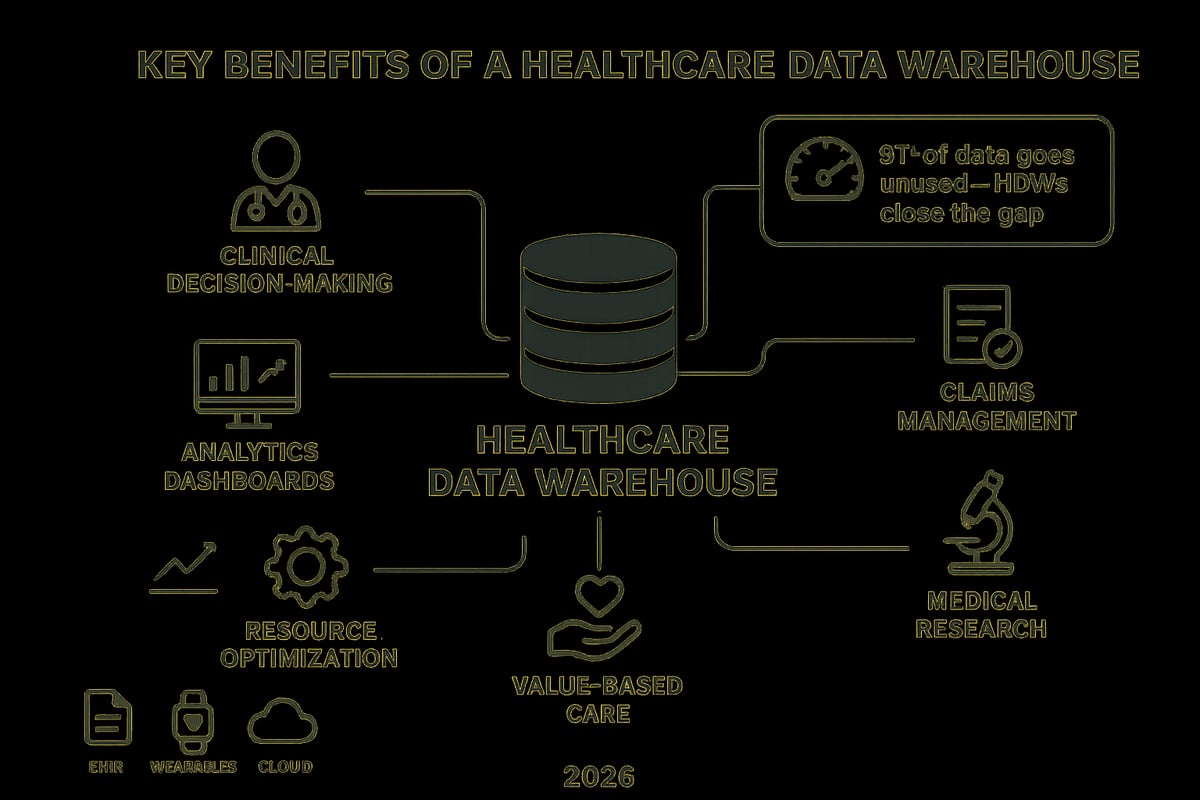
Improved Clinical Decision-Making
A healthcare data warehouse brings together data from EHRs, lab systems, and wearables, creating a unified patient record. This comprehensive view enables clinicians to make evidence-based decisions at the point of care. Real-time access to complete patient histories helps reduce errors and avoid unnecessary tests.
Currently, up to 97 percent of healthcare data is unused. By leveraging a healthcare data warehouse, providers can bridge this gap, ensuring that every relevant data point informs patient care. This leads to safer, more accurate diagnoses and improved treatment outcomes.
Enhanced Reporting and Analytics
Timely, accurate analytics are essential for effective healthcare management. A healthcare data warehouse streamlines reporting by aggregating structured data into standardized formats. Clinicians and administrators can monitor performance, track quality measures, and identify trends with ease.
Interactive dashboards provide rapid insights into costs, patient cohorts, and outcomes. This empowers organizations to benchmark performance, highlight areas for improvement, and support data-driven decision-making at every level.
Optimized Resource and Cost Management
Healthcare resources are limited, making efficient allocation crucial. A healthcare data warehouse enables leaders to analyze utilization patterns, forecast demand, and identify high-risk or high-cost patients early.
Data-driven insights help reduce unnecessary spending and direct resources where they are needed most. By identifying inefficiencies and tracking interventions, organizations can optimize workflows and reduce operating costs.
Support for Value-Based Care and Population Health
The shift toward value-based care rewards measurable improvements in patient outcomes. A healthcare data warehouse makes it possible to design personalized care plans by integrating clinical, claims, and social determinants data.
Providers can target interventions for specific populations, monitor progress, and demonstrate improvements in satisfaction and health outcomes. This supports compliance with quality programs and advances population health goals.
Streamlined Claims and Revenue Cycle Management
Managing claims efficiently is vital for financial sustainability. A healthcare data warehouse automates claims processing, reduces manual errors, and accelerates reimbursement cycles. Advanced analytics also support fraud detection and prevention.
For healthcare providers seeking to efficiently recover underpayments, a robust data warehouse ensures accurate, timely claims and minimizes revenue leakage. This leads to improved cash flow and stronger financial performance.
Accelerated Medical Research
Research teams benefit from access to large, cleansed datasets spanning multiple sources. A healthcare data warehouse supports clinical studies, comparative effectiveness research, and rapid data sharing across institutions.
Collaboration is enhanced, enabling faster discoveries and broader participation in research initiatives. Examples like the WHO Global Health Observatory and Ukraine’s National Clinical Data Repository showcase the transformative power of healthcare data warehousing on a national and global scale.
Essential Features of a Modern Healthcare Data Warehouse
Modern healthcare data warehouse solutions are built to handle the complexity, scale, and regulatory demands of 2026. Healthcare organizations rely on these robust systems to unify data, support compliance, and drive innovation in care delivery. Understanding the essential features is critical for any leader seeking to maximize value from their healthcare data warehouse investment.
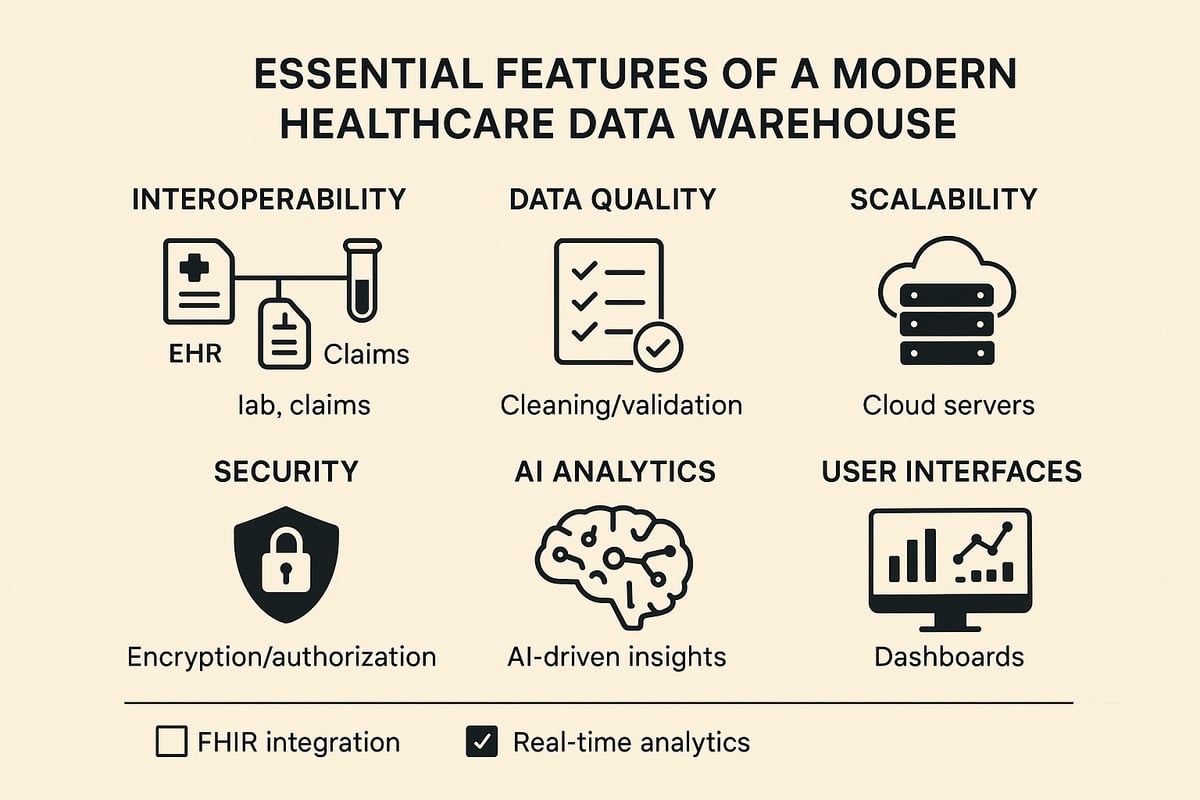
Data Integration and Interoperability
A leading healthcare data warehouse must seamlessly connect diverse data sources. These include EHRs, ERPs, lab systems, insurance databases, and external data feeds. True interoperability is achieved when data flows easily and accurately between systems, breaking down silos that hinder care coordination.
Support for healthcare data standards, such as FHIR, is now essential. FHIR enables structured, consistent data exchange, making it easier to share insights across organizations and platforms. As FHIR Adoption in Healthcare Interoperability highlights, FHIR-first architectures are rapidly becoming the industry benchmark for data sharing and ecosystem integration.
A healthcare data warehouse with strong interoperability accelerates collaboration and supports national and global health initiatives.
Data Quality, Cleansing, and Validation
Data quality is foundational for any healthcare data warehouse. Automated processes for data cleansing and validation are essential to ensure that information is accurate, complete, and consistent. These processes detect and remove duplicates, correct errors, and standardize terminology, reducing the risk of faulty analytics.
For example, a modern healthcare data warehouse will flag invalid entries and reconcile conflicting data from multiple sources. This level of rigor empowers clinicians and administrators to trust the insights they derive, improving outcomes and compliance.
Scalability and Performance
As healthcare data volumes grow exponentially, scalability becomes a defining feature of any healthcare data warehouse. Cloud-native architectures are preferred for their elasticity, allowing organizations to scale resources up or down based on demand.
Performance is equally crucial. A high-performing healthcare data warehouse supports both real-time and batch processing, ensuring that analytics and reporting are always timely. This responsiveness is vital for population health management, research, and operational efficiency.
Security and Compliance
Protecting sensitive health information is non-negotiable. A healthcare data warehouse must include robust security measures, such as encryption, role-based access controls, and comprehensive audit trails. These features safeguard patient privacy and protect against breaches.
Compliance with evolving regulations, including HIPAA and GDPR, is mandatory. Advanced features like Attribute-Based Access Control (ABAC) and data pseudonymization provide layered defenses for sensitive data, meeting the strictest standards for healthcare organizations.
Advanced Analytics and AI Integration
The modern healthcare data warehouse is more than a data repository. It is a platform for advanced analytics and artificial intelligence. Built-in support for machine learning, predictive modeling, and data mining turns raw data into actionable insights.
These capabilities enable real-time risk stratification, early disease detection, and proactive resource allocation. During public health crises, AI-powered analytics in a healthcare data warehouse can identify emerging threats, supporting rapid response and mitigation.
User-Friendly Interfaces and Reporting Tools
Accessibility is a hallmark of a high-performing healthcare data warehouse. Self-service dashboards empower clinicians and administrators to explore data without relying on IT specialists. Customizable reporting tools allow users to generate insights tailored to their roles and objectives.
Modern interfaces are intuitive and responsive, reducing barriers to adoption and fostering a data-driven culture. Solutions like Kodjin FHIR Server offer robust validation and interoperability, while Arcadia’s analytics dashboards exemplify the power of user-centric design in healthcare data warehouse platforms.
| Feature | Benefit |
|---|---|
| Interoperability (FHIR support) | Seamless data exchange, reduced silos |
| Data Quality and Validation | Trustworthy insights, better decisions |
| Scalability and Performance | Handles large, diverse datasets efficiently |
| Security and Compliance | Protects privacy, ensures regulatory fit |
| Advanced Analytics and AI | Predictive, actionable intelligence |
| User-Friendly Dashboards | Broad accessibility, faster adoption |
Major Challenges in Healthcare Data Warehousing
Healthcare organizations face a range of obstacles when implementing and maintaining a healthcare data warehouse. As data volumes surge and expectations for actionable insights grow, these challenges can hinder progress, increase risk, and limit the value of data-driven initiatives.
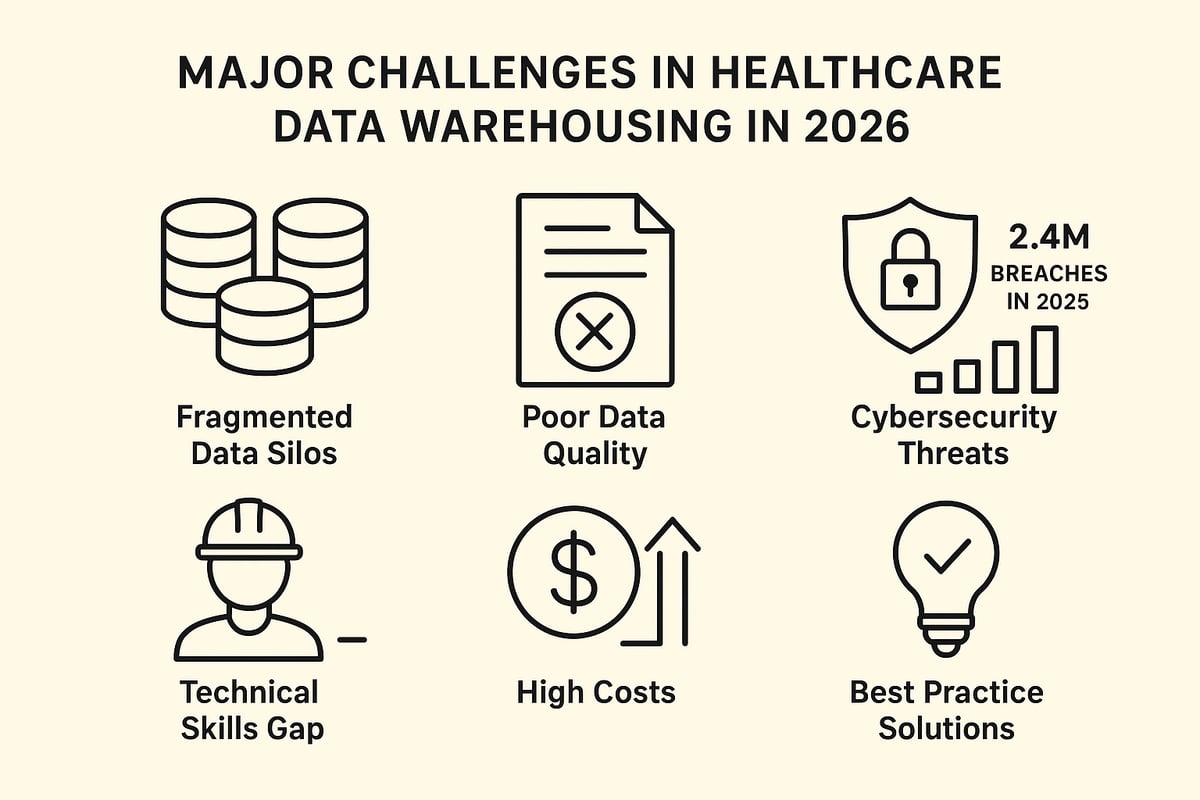
Data Silos and Interoperability Barriers
Many healthcare organizations still operate with data scattered across electronic health records, lab systems, and third-party platforms. Each system may use different formats, making integration with a healthcare data warehouse complex.
This fragmentation leads to silos, where critical patient or operational data remains locked in isolated systems. As a result, organizations struggle to create a unified view of their data, limiting analytics and decision-making capabilities.
Interoperability issues persist, even as standards like FHIR gain traction. Without seamless data exchange, the full potential of a healthcare data warehouse remains out of reach.
Data Quality and Integrity Issues
Ensuring high-quality data is foundational for any healthcare data warehouse. However, challenges such as missing fields, outdated records, and inconsistent terminology are common.
When data comes from multiple sources, discrepancies in coding and formatting can undermine accuracy. Duplicate entries or invalid data further complicate analytics, leading to unreliable results.
Ongoing data validation and cleansing are essential. Without these processes, healthcare data warehouse initiatives risk propagating errors throughout the organization.
Security Threats and Compliance Risks
The healthcare sector is a prime target for cybercriminals, with the value of sensitive patient data attracting sophisticated attacks. In 2024, 80 percent of healthcare organizations reported attempted breaches, highlighting escalating risks.
A healthcare data warehouse must safeguard information through encryption, access controls, and continuous monitoring. Regulatory compliance is equally critical, as violations of HIPAA or GDPR can result in steep penalties. According to Healthcare Data Breach Statistics 2025, the frequency and scale of breaches continue to rise, underscoring the urgent need for robust security frameworks.
Ukraine’s National Clinical Data Repository addresses these concerns with electronic signatures and attribute-based access control, ensuring both data integrity and compliance.
Technical Complexity and Skills Gaps
Building and maintaining a healthcare data warehouse requires specialized technical expertise. Organizations must design scalable architectures, manage complex data pipelines, and ensure real-time analytics capabilities.
The shortage of skilled professionals in healthcare IT and data management further complicates these efforts. This skills gap can delay deployments, increase costs, and limit innovation.
Ongoing training and investment in talent are essential to maximize the value of a healthcare data warehouse and keep pace with evolving technologies.
Cost and Resource Constraints
Implementing a healthcare data warehouse involves significant upfront investment in infrastructure, software, and skilled personnel. These costs can be a barrier for many organizations, particularly smaller providers or those with limited budgets.
Ongoing expenses, such as system maintenance, upgrades, and compliance monitoring, add further complexity. Resource constraints may lead to compromises in scope or quality, reducing the effectiveness of the healthcare data warehouse.
Strategic planning and phased rollouts can help organizations manage costs while still achieving long-term goals.
Solutions and Best Practices
To overcome these challenges, organizations often partner with experienced vendors who offer proven healthcare data warehouse solutions and support. Adopting modular, scalable architectures allows for gradual expansion and reduces risk.
Continuous training and upskilling of staff help close the expertise gap. Strong data governance frameworks, coupled with best-in-class security measures, ensure compliance and data integrity.
By following these best practices, organizations can unlock the full value of their healthcare data warehouse and drive better outcomes across clinical, operational, and financial domains.
Leading Healthcare Data Warehouse Models and Architectures
Choosing the right healthcare data warehouse model is pivotal for healthcare organizations aiming to maximize data utility, ensure compliance, and drive innovation. The landscape in 2026 features several architectures, each tailored to specific organizational needs, from enterprise-wide governance to rapid departmental agility.
Enterprise Data Model
The enterprise data model is a top-down approach, standardizing data organization and definitions across the entire healthcare data warehouse. This model fosters consistency, governance, and reliability, making it ideal for large healthcare systems with complex regulatory requirements.
A centralized structure streamlines analytics and supports advanced use cases, such as system-wide performance monitoring and compliance reporting. Strong data governance is essential for this model, as highlighted in Data Governance in Healthcare Analytics.
Independent Data Mart Model
The independent data mart model takes a bottom-up approach. Here, individual departments or business units create their own data marts, each tailored to specific analytic needs. Later, these marts can be integrated to form a broader healthcare data warehouse.
This model offers flexibility and speed, allowing departments to respond rapidly to evolving requirements. However, without careful management, it can result in data silos and inconsistencies, challenging interoperability and system-wide analytics.
Hybrid Model
The hybrid model blends enterprise-wide standards with the flexibility of departmental data marts. It enables organizations to maintain governance and consistency while accommodating unique departmental needs within the healthcare data warehouse.
Departments can innovate and adapt quickly, while the enterprise layer ensures data quality, security, and interoperability. This balance makes the hybrid model popular among organizations seeking both agility and robust oversight.
Cloud-Based and Federated Models
Cloud-based healthcare data warehouse architectures leverage scalable, secure cloud infrastructure. They enable organizations to manage large volumes of data efficiently and cost-effectively, supporting both real-time and batch processing.
Federated models allow data to remain at its source, rather than being physically consolidated. This approach enhances privacy, reduces duplication, and supports collaboration across different entities, such as hospitals, research groups, or national repositories.
Open-Standard and FHIR-First Architectures
Open-standard and FHIR-first architectures prioritize interoperability across the healthcare data warehouse ecosystem. By using standards like FHIR and HL7, these models support seamless data exchange with external partners, health networks, and national databases.
This approach accelerates integration, enables advanced analytics, and supports compliance with global health data initiatives. It is especially valuable for organizations participating in cross-border research or nationwide health programs.
Case Studies
Real-world examples highlight the value of these models. The WHO Global Health Observatory exemplifies a global-scale, theme-based healthcare data warehouse, supporting international analytics and policy decisions.
Ukraine’s National Clinical Data Repository leverages a FHIR-based architecture to ensure secure, interoperable, and scalable data management. Both demonstrate how the right architecture can drive impactful outcomes, streamline operations, and foster collaboration.
Real-World Applications and Future Trends
Healthcare organizations in 2026 are experiencing a wave of innovation, thanks to advances in the healthcare data warehouse. These platforms are transforming how data is used, driving improvements across clinical, operational, and financial domains.
Use Cases in 2026
The healthcare data warehouse is central to population health management, predictive analytics, and patient engagement. Providers use these systems to identify at-risk populations, automate care management, and deliver personalized interventions.
Wearables and IoT devices feed real-time patient data into the healthcare data warehouse, enabling proactive monitoring of chronic conditions. Automated alerts and dashboards help clinicians act quickly, improving patient outcomes.
Financial teams also benefit. By leveraging analytics from the healthcare data warehouse, organizations can optimize billing workflows and reduce revenue leakage. For example, streamlining your billing process is a practical outcome, with data-driven insights reducing errors and delays.
Advanced Analytics and AI
Modern healthcare data warehouse solutions are built for advanced analytics. AI and machine learning models process vast datasets to forecast disease outbreaks, predict patient deterioration, and recommend tailored therapies.
Natural language processing (NLP) tools unlock the value in clinical notes and unstructured records, extracting insights that were previously hidden. With the healthcare data warehouse as the foundation, organizations gain a comprehensive view of patient and population health.
These capabilities accelerate research and support rapid decision-making. Early warning systems powered by AI can identify public health threats before they escalate.
Integration with National and Global Health Initiatives
The healthcare data warehouse plays a pivotal role in supporting government reporting, quality initiatives, and clinical research. National repositories such as Ukraine’s National Clinical Data Repository and the WHO Global Health Observatory rely on integrated data for effective surveillance and response.
Cross-border data sharing, made possible by interoperable healthcare data warehouse architectures, strengthens pandemic preparedness and health equity efforts. Organizations can contribute to global studies while maintaining compliance and security.
By aligning with international standards, the healthcare data warehouse ensures seamless data exchange and collaboration at scale.
Future Directions
Looking ahead, the healthcare data warehouse will expand to incorporate more patient-generated data, including mobile apps and connected devices. This evolution will enhance patient engagement and enable more precise, real-time interventions.
Privacy, consent, and data ethics will become even more important. Enhanced security measures and transparent governance will be essential as data volumes grow.
Automation, including robotic process automation (RPA), will streamline repetitive tasks and help organizations adapt quickly to regulatory changes. Ukraine’s NCDR and WHO GHO offer blueprints for future-ready healthcare data warehouse strategies.
Steps to Implement a Healthcare Data Warehouse in 2026
Implementing a healthcare data warehouse in 2026 requires a strategic, phased approach. Each step builds a foundation for secure, efficient, and value-driven data management. By following these best practices, organizations can improve outcomes, streamline operations, and stay compliant.
Step 1: Define Objectives and Stakeholders
Begin by aligning your healthcare data warehouse project with the organization’s clinical, financial, and research goals. Identify all key stakeholders, including clinicians, IT specialists, compliance officers, and administrators. This ensures every perspective is considered from the outset, promoting buy-in and clarity of purpose.
Step 2: Assess Data Sources and Integration Needs
Inventory all existing systems, such as EHRs, lab databases, claims platforms, and external data feeds. Understanding the variety and format of data sources is crucial for seamless integration. Early planning for interoperability minimizes future disruptions and supports scalability.
Step 3: Select the Right Architecture and Technology
Choose the most suitable architecture—whether enterprise, data mart, hybrid, or cloud/federated models. Prioritize platforms that support FHIR and other interoperability standards. Cloud-native solutions offer flexibility, while technologies like Kodjin’s FHIR Server can accelerate secure integration and future-proof your investment.
Step 4: Ensure Data Quality and Governance
Establish robust processes for data cleaning, validation, and deduplication. High-quality data is the backbone of any healthcare data warehouse, directly impacting analytics and patient care. Addressing common medical billing mistakes at this stage helps maintain data integrity and prevents costly errors down the line.
Step 5: Build Security and Compliance into the Design
Incorporate security measures like encryption, access controls, and audit trails from the outset. Compliance with HIPAA, GDPR, and local regulations is non-negotiable. Attribute-Based Access Control (ABAC) and pseudonymization are essential for protecting sensitive health information in your healthcare data warehouse.
Step 6: Develop Analytics and Reporting Capabilities
Deploy dashboards, self-service reporting tools, and AI-powered analytics to turn raw data into actionable insights. Training users and fostering a data-driven culture are critical for adoption. Addressing common healthcare underpayment issues through accurate reporting can improve revenue cycle management and operational efficiency.
Step 7: Plan for Scalability and Ongoing Optimization
Opt for scalable, cloud-native solutions that can grow with your organization’s needs. Continuously monitor warehouse performance, adapt to new data sources, and update processes to stay ahead of regulatory changes. Reference platforms like Arcadia’s, which handle large-scale data integration and analytics, for guidance on sustainable growth.
By following these seven steps, healthcare organizations can successfully implement a healthcare data warehouse that drives better clinical decisions, optimizes costs, and maintains compliance in an evolving digital landscape.

